Category Archives: Updates
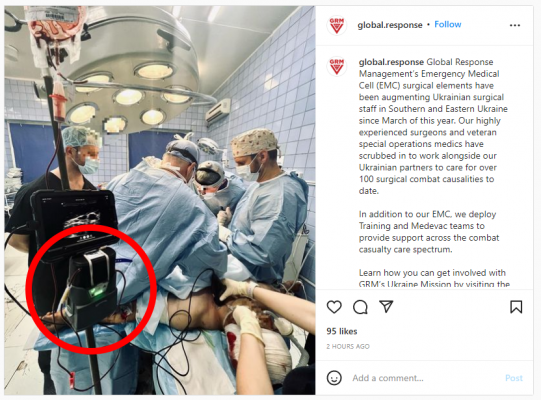
Warrior lite is used to help saving lives in Ukraine!
A picture is worth a thousands words… We are proud that our Warrior lite has [...]
Jun
COVID: Weak Points Exposed and Lessons Learned
Saying that the past two years have been unpredictable is an understatement. In the winter [...]
Nov
“The patient survived a non-survivable gunshot wound to the chest!”
How often does a company have the opportunity to contribute to an ‘impossible’ recovery of [...]
Prehospital Transfusion of Low-Titer O + Whole Blood for Severe Maternal Hemorrhage: A Case Report
Access full study in PubMed Ryan Newberry, C J Winckler, Ryan Luellwitz, Leslie Greebon, Elly Xenakis, William Bullock, Michael Stringfellow, Julian Mapp PMID: 31550184 [...]
3 takeaways from the recent TCCC guidelines for the management of hypothermia in tactical combat casualty care
The recent TCCC guidelines TCCC guidelines for the management of hypothermia in tactical combat casualty care [...]
Warrior superiority recognized in TCCC Guidelines for Management of Hypothermia in Tactical Combat Casualty Care
PLANO, September. 25, 2020 – QinFlow, the manufacturer of the Warrior, a modular blood and IV [...]
Accident Survivor, Military Family Finally Able to Donate Blood
BY BRYAN BOES SAN ANTONIOPUBLISHED 6:16 AM CT JUL. 06, 2020FULL ARTICLE Spectrum News SAN ANTONIO – A recent decision [...]
FDA Updates to Bring in New Blood Donors Starting July 1 at South Texas Blood & Tissue Center
FULL ARTICLE South Texas Blood & Tissue Center June 30, 2020 at 5:04 pm CDT [...]
Resident Eagle: Whole Blood in the Rural EMS Environment
EMS World Issue: July 2020 Casey Ebrom, EMT-P, FP-C; Craig Manifold, DO, FACEP, FAAEM, FAEMS; and [...]
From battlefront to homefront: creation of a civilian walking blood bank
Published by STRAC Supplement Article, Online Library FULL ARTICLE Maxwell A. Braverman, Alison Smith, Charles [...]