Blood Warming, General, Whole Blood
Why Does Blood Need to Be Warmed?
I’m a big believer in knowing why you are doing something and not just following blindly because your protocols tell you to. In this article I’m going to talk about why we warm blood before giving it to patients. The World Health Organization strongly recommends warming blood products when they are given at rates at and above 100mL/min. We can cause serious harm to our patients, even cardiac arrest, when we infuse cold blood. While cardiac arrest is a rare consequence of cold transfusions, hypothermia is not. In fact, up to 66% (2 out of 3) trauma patients are hypothermic upon admission to the hospital. That’s an alarming number that I think we as prehospital care providers can change for the better.
Let’s think about our trauma patient for a second. We arrive on scene to find a person who has been in a car accident, or shot, or fell off a ladder. Regardless of the mechanism of injury, what we know for sure is that they have been in this condition for some period of time (unless you witnessed the accident happen in front of you). What’s the average response time of your agency? If you work in a rural or remote area, it could be an hour or even longer before you arrive on scene. During this time your patient is being exposed to the elements. Even in warm temperatures, trauma patients can become hypothermic quickly. And if your trauma patient is hypovolemic due to blood loss, they are losing the ability to retain what heat they have.
Now let’s consider the path our trauma patient is going to take on their road to recovery. We as prehospital providers are going to provide care in the field by stabilizing the patient’s injuries and starting the resuscitation process by obtaining IV access and infusing blood products. Then we are going to transport them to the nearest appropriate facility where they will continue their journey to recovery. Keep in mind our transport time is probably going to be as long as our response time. Finally, once at the hospital, trauma teams will expose the patient again to do their own assessment. The patient may require surgery also. This means being exposed in a cold OR and being put under by anesthesia. (Note that anesthesia impacts the body’s ability to thermoregulate.) Then our patient will spend time in PACU and finally ICU.
That’s a long time for your trauma patient to be without warmed blood. We as providers can stop this from occurring by limiting exposure and warming blood products before they are infused into the patient. Trauma patients that are admitted to the ICU with hypothermia have a significantly greater risk of mortality than those patients who are normothermic upon arrival (Balvers 2016). We as prehospital providers can set our patients up for the best possible odds of survival by keeping them warm. One way we can do this is simply by limiting the amount of time the patient is exposed. Keep the patient covered with heat reflective blankets when not actively assessing the patient. The other way we can prevent hypothermia in our trauma patients is to ensure that we warm blood products, which are stored in coolers at near-freezing temperature, prior to infusing them to patients.
So that’s the first reason we warm blood before giving it to our patients, to help in preventing hypothermia. Another reason we need to warm blood before infusing is because blood doesn’t work when it’s cold. What do I mean by this? The function of blood is to carry oxygen to our tissues and remove waste products. Blood also clots to prevent excess bleeding when vessel damage occurs. However, the enzymes that carry out these functions can’t work when blood is cold. Blood is stored near freezing to prevent growth of bacteria and to increase shelf life, but the life-giving functions of blood only work when blood is warmed back to body temperature.
The way oxygen is transported through our body is by attaching to hemoglobin within red blood cells. When red blood cells circulate through the pulmonary arteries, the oxygen diffuses into the blood and attaches to hemoglobin. When blood circulates to tissues that are in need of oxygen, the oxygen molecules leave the hemoglobin molecule and diffuse into the cells that need it. There are several factors that affect how well oxygen binds to hemoglobin. These same factors affect how well hemoglobin offloads oxygen to cells that need it.
This relationship can be visualized by the oxyhemoglobin dissociation curve. That’s a fancy sounding name but don’t let it intimidate you. The curve, shown below, has the amount of oxygen (measured in partial pressure) on the horizontal axis and the saturation (percentage) of hemoglobin on the vertical axis. As the amount of oxygen increases, so does the percentage of saturated hemoglobin. When red blood cells pass through the lungs, you want hemoglobin to have a high affinity for oxygen. When blood reaches the tissues that need oxygen, you want hemoglobin to have less affinity for oxygen.
Factors that affect this phenomenon include temperature and pH among others. At increased temperatures, hemoglobin holds on to oxygen less tightly. The heat produced by metabolism in cells causes the hemoglobin to bind less tightly and therefore offload the oxygen to tissues that need it. Now what happens if we cool things down by infusing cold blood? Well the oxygen is going to stay stuck to hemoglobin and not go to the cells that need it like your heart, liver, kidneys, and brain. This is one very important reason we warm blood, especially when bolusing it.
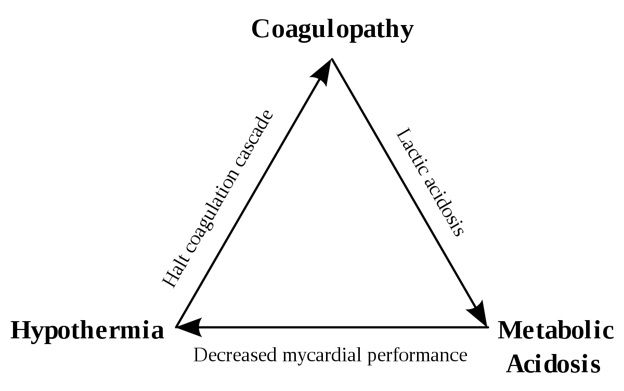
This brings us to our third reason we warm blood products; clotting factors. The way our blood clots is described by the clotting cascade. I’m not going to get into details, but just know that it requires several different enzymes, all to function properly, in order to clot. Most enzymes have a physiologic range at which they perform best. Those conditions are usually at normothermic temperatures (38), and physiologic pH (7.35-7.45). Outside of these parameters, enzyme activity suffers, and clotting factors are no different. At hypothermic temperatures, clotting factor activity decreases. This results in more blood loss, and more heat loss, less oxygen carrying capacity and eventually death if not corrected.
These three factors; hypothermia, coagulopathy, and acidosis make up what is known as the trauma triad or lethal triad. The lethal triad shows the relationship between these three conditions and how one propagates the other. However, when one side is corrected, the other two sides of the triangle are also corrected. Thus, when we combat hypothermia by first warming blood products before administering them, we are also helping to correct acidosis and coagulopathy.
I hope that by now you have a good idea of why you need to warm blood before giving it to the patient, especially when giving in rapid, mass transfusions. The more we know as prehospital providers, the better we can treat our patients and improve their odds of survival. By warming blood, we increase the oxygen delivering capabilities of red blood cells. We also ensure that the clotting factors are able to function properly and help control bleeding.
If your agency is thinking about starting to carry blood products (which is an excellent idea in my opinion), you also need a warmer that is up to the job. QinFlow’s line of Warrior and Warrior lite warmers are the ideal solution for the pre-hospital and inter facility setting. They also make products that work in the ER/OR settings, all while using the same consumable, to eliminate waste and transition from one warmer to another seamlessly. QinFlow’s consumables are 100 percent aluminum free and utilize a simple design free of microchips. The former eliminates aluminum toxicity concerns (read my article “Aluminum: The Hidden Danger in Blood Warmers”) while the latter ensures affordable per-use price as well as product availability to meet demand, a major issue that has surfaced during COVID (read my article “COVID: Weak Points Exposed and Lessons Learned”).
Balvers K, Van der Horst M, Graumans M, et al. Hypothermia as a predictor for mortality in trauma patients at admittance to the Intensive Care Unit. J Emerg Trauma Shock. 2016;9(3):97-102. doi:10.4103/0974-2700.185276
Ghosh I, Haldar R (2019) Blood warming in trauma related transfusions-Precepts and practices. J Cardiovasc Med Cardiol 6(4): 094-097. DOI: 10.17352/2455-2976.000101